A complex medical term, asthenoteratozoospermia, is a concerns couples struggling with infertility issues. This condition indicates low sperm vitality or even malformation and according to a study, occurs in 1 out of 5000 men. Many couples are curious about the diagnosis and how asthenoteratozoospermia can affect their journey to parenthood. In this blog, we’ll explain the medical jargon’s causes, symptoms, and treatments to make it easier for you to understand and help you find solutions.
Asthenoteratozoospermia – Understanding The Medical Term
One of the main reasons for male infertility is asthenozoospermia (AZS), characterized by decreased or insufficient sperm motility.This prevents the sperm from moving around to reach the egg and fertilize it. As a result, this condition makes it difficult for a couple to conceive. The ejaculated sperm must pass through the cervical mucus to reach the female uterus. To fertilize the ovum, it should eventually pierce through the egg after entering the uterus.
Asthenoteratozoospermia – Learning The Causes, Symptoms And Treatments
You may also be wondering whether this condition is curable. Well, to answer this question, yes, asthenoteratozoospermia is curable. Let’s have a look at the asthenoteratozoospermia treatment in detail.
Asthenoteratozoospermia – Causes
Asthenozoospermia can be caused by a variety of factors, including those listed below:
Lifestyle changes:
An unhealthy diet might impact the mobility of sperm. For instance, smoking, excessive alcohol consumption, and drug usage lower your testosterone and can all contribute to the condition. Men who work in occupations that repeatedly injure the pelvic region, such as driving a car or riding a horse, are also at risk for asthenozoospermia.
Seminal fluid-related infections:
The ability of sperm to fertilize the egg can be affected by illnesses that affect the male reproductive system. Orchitis, epididymitis, prostatitis, and vesiculitis seminal can be brought on by infections of the urethra, prostate, ejaculatory ducts, seminal vesicles, and more brought on by sexually transmitted conditions like gonorrhea or chlamydia.
Immunological components:
Various antibodies may function as a barrier to your sperm’s travel in different ways. Numerous studies have demonstrated that your sperm’s tails contain anti-sperm antibodies, which prevents them from fertilizing the egg.
Acute heatstroke in the scrotum:
The scrotum, or sac surrounding the testicles, becomes hotter, which changes the quality of the semen. Low sperm count is related to testicular overheating. Wearing tight briefs rather than boxers and taking extremely hot showers, baths, or saunas are contributing factors. The testicles can also overheat from a lack of exercise and some occupations, such as driving a cab or constantly sitting with a laptop on your lap.
Radiotherapy and chemotherapy:
Radiation therapy, often known as radiotherapy or chemotherapy, kills cancer cells. The issue is that they also harm healthy cells that divide quickly. Each form of therapy has its own outcomes. When combined, you may experience adverse effects from both therapies, which is common. Because of this, the production of healthy sperm may decrease or perhaps stop entirely.
Other common causes of asthenozoospermia include – Varicocele, chromosome abnormalities, age, exposure to toxic products, vasectomy, genetic predispositions, or underlying medical conditions.
Read Also: Understanding Sperm Cramps: Causes, Symptoms, and Treatment Options
Asthenoteratozoospermia Symptoms
Multiple unsuccessful attempts to conceive are the first, and possibly already late, indicators of asthenoteratozoospermia. But even here, the situation might be complicated. There are some other symptoms of asthenozoospermia as well, including –
- A very small number of sperm with good motility
- Thickening and expansion of the scrotum’s veins
- Fluid surrounding the testicles with hydrocele or pyocele that is hypoechoic or anechoic
- Having hormonal imbalances
- Pelvic or urinary pain
Read Also: Understanding Male Fertility: A Comprehensive Guide to In terpreting Semen Analysis Reports
Asthenoteratozoospermia Treatment
There are numerous Asthenoteratozoospermia treatments available for men. An effort is made to stop the negative activities that cause it, like lifestyle patterns.
A healthier lifestyle:
Changing one’s lifestyle to one that is healthy and refraining from harmful practices like smoking, drinking alcohol, and abusing drugs—habits that degrade sperm quality overall—are some recommendations for those with these conditions.
Good diet and food choices:
Doctors also advise eating foods high in vitamins, such as zinc. If the fertility issue is due to some infection, the patient is given antibiotic prescriptions, and the study is repeated approximately three months later to assess the treatment outcome.
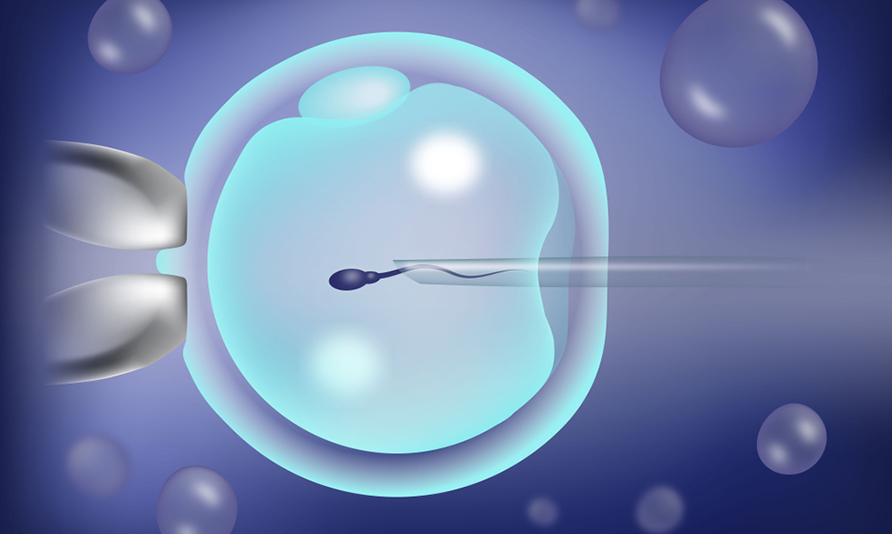
ICSI (intracytoplasmic sperm injection):
Sperm must get inside the egg for fertilization to happen. Sometimes, the outer layer prevents the sperm from penetrating. The sperm is injected directly into the egg during a procedure known as intracytoplasmic sperm injection (ICSI), which can aid in fertilization. To achieve fertilization using this approach, a single sperm is injected into an adult oocyte. It is one of the assisted reproductive techniques (ART) most frequently used to address male infertility issues.
Traditional IVF:
This method can be used when an asthenozoospermia is minimal. It is the simplest form of IVF and involves infusing the egg with many sperm to facilitate fertilization. It is a method of treating infertility in which sperm fertilize a woman’s eggs (called oocytes) in a laboratory dish. After being placed in the woman’s uterus, one or more fertilized eggs (embryos) will implant and result in a pregnancy.
IUI, or intrauterine insemination:
The process includes gathering and sanitizing the sperm. A fine plastic tube is then used to implant the sperm traveling the fastest into the womb. Its benefits in male and cervical factor infertility include sperm bypassing potentially harmful cervical factors and an increase in the number of sperm that enter the uterine canal. However, this approach is only advised if the female spouse is younger than 35 and is not experiencing reproductive problems.
Start Your Journey TO Parenthood With The Best: Nandi IVF
Male infertility issues like asthenozoospermia, have several treatable causes. Assisted reproductive techniques can increase a couple’s chances of conceiving. They consist of fertility medications, medical equipment, surgery, or various procedures. At Nandi IVF, we give you proper insight into fertility related issues and assist you navigate through them. We have a team of skilled doctors to guide you at all stages of pregnancy, from conceiving to bringing a new life into the world. Contact us and start your journey to parenthood.
FAQs:
Q: What is asthenozoospermia?
Ans: Asthenospermia, another name for asthenozoospermia, is a change that impacts sperm motility. It is also referred to as inactive sperm or sperm that moves slowly. Because the sperm cells lack the necessary motility to reach the egg and achieve fertilization, it is a cause of infertility in men.
Q: Is asthenozoospermia curable or not?
Ans: Yes, asthenozoospermia is curable. From mild to severe cases, asthenozoospermia can be cured by medications, lifestyle changes, or surgery.
Q: What is teratozoospermia?
Ans: Teratozoospermia is a sperm condition where men’s ejaculated sperm are deformed or improperly produced, which affects fertility. Infertility results from poorly shaped sperm because they may not reach the egg or be strong enough to fertilize the egg within a woman, resulting in teratozoospermia.
Q: What is the natural cure for asthenozoospermia?
Ans: The natural cure for asthenozoospermia should be to change one’s lifestyle and behaviors, such as quitting smoking, drinking alcohol, using drugs, exercising more, maintaining a healthy weight, eating a balanced diet, etc.
Q: What does asthenozoospermia mean?
Ans: The sperm’s incapacity to move effectively within a woman’s body is essential for it to reach the egg and generate a pregnancy. Thus, sperms with lower motility (movement) relative to healthy ones are said to have asthenozoospermia.
Q: Is there any treatment for teratozoospermia?
Ans: Yes, teratozoospermia can be treated by lifestyle changes like exercising, eating a healthy diet, quitting drugs, alcohol, and smoking. Medications, surgery, supplements, and Assisted Reproductive Technology are also helpful in treating teratozoospermia.
Q: What Asthenospermia signs & symptoms are there?
Ans: The symptoms of Asthenospermia include- trouble getting pregnant, hormonal imbalances, low sperm count, and more. To make a diagnosis, a semen analysis is required.
Read Also: Comparing Tubectomy and Vasectomy: Which Option is Right for You?